FROZEN SHOULDER
Adhesive Capsulitis
Adhesive Capsulitis (Frozen shoulder) is characterized by pain and loss of motion or stiffness in the shoulder. It affects about two percent of the general population. Frozen shoulder most commonly affects patients between the ages of 40 and 60 years, with no clear predisposition based on sex, arm dominance, or occupation.
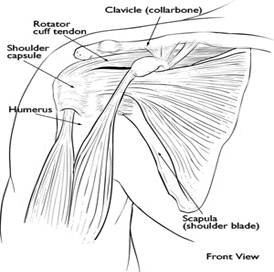
Cause The causes of frozen shoulder are not fully understood. The process involves thickening and contracture (tightening) of the capsule surrounding the shoulder joint. There are some conditions which are associated with the development of frozen shoulder.
Frozen shoulder inioccurs much more commonly in individuals with diabetes, affecting 10 percent to 20 percent of these individuals. Other medical problems associated with increased risk of frozen shoulder include: hypothyroidism, hyperthyroidism, Parkinson’s disease, and cardiac disease or surgery.
Frozen shoulder can develop after a shoulder is immobilized for a period of time. Attempts to prevent frozen shoulder include early motion of the shoulder after it has been injured.
Symptoms
Pain due to frozen shoulder is usually dull or aching. It can be worsened with attempted motion. The pain is usually located over the outer shoulder area and sometimes the upper arm. However, without use or motion the shoulder may be completely pain free.
The hallmark of the disorder is restricted motion or stiffness in the shoulder in all directions. The affected individual cannot move (active motion) the shoulder normally. Motion is also limited when someone else attempts to move (passive assist) the shoulder for the patient. A frozen shoulder may have three stages:
Stage one: In the “freezing” stage, the patient develops a slow onset of pain. As the pain worsens, the shoulder loses motion. This stage may last from six weeks to nine months.
Stage two: The “frozen” stage is marked by a slow improvement in pain, but the stiffness remains. This stage generally lasts four months to nine months.
Stage three: The final stage is the “thawing,” during which shoulder motion slowly returns toward normal. This generally lasts five months to 26 months.
Diagnosis
A doctor can diagnose frozen shoulder based on the patient’s symptoms and a physical examination. X-rays or MRI (magnetic resonance imaging) studies are sometimes used to rule out other causes of shoulder stiffness and pain, such as a rotator cuff tear. Therefore, in frozen shoulder studies are usually normal.
Treatment
Frozen shoulder will generally get better on its own. However, this takes some time, occasionally up to two to three years. Treatment is aimed at pain control and restoring motion.

Nonsurgical Treatment
Pain control can be achieved with anti-inflammatory medications. These can include pills taken by mouth, such as ibuprofen, or by injection, such as corticosteroids.
Physical therapy is used to restore motion. This may be under the direct supervision of a physical therapist or via a home program. Frozen shoulder therapy includes stretching or range-of-motion exercises for the shoulder. Sometimes, heat is used to help decrease pain. If these methods fail, injections are sometimes used to limit pain and allow more aggressive physical therapy.
More than 90 percent of patients improve with these relatively simple treatments. Usually, the pain resolves and motion improves. However, in some cases, even after several years the motion does not return completely and a small amount of stiffness remains.
Surgical Treatment
Surgical intervention is considered when there is no improvement in pain or shoulder motion after an appropriate course of physical therapy and anti-inflammatory medications. When more invasive measures are considered, the patient must always consider that most individuals will get better if given sufficient time and that surgery always has risk involved. Manipulation under anesthesia involves putting the patient to sleep and forcing the shoulder to move. This process causes the capsule to stretch or tear.
Contact Us
13710 Olive Boulevard (Primary Office)
Chesterfield, MO 63017
Telephone: 314-469-PAIN (7246)
Fax: 314-469-7251
Exchange: 314-441-6965 (for after-hour Emergencies Only)
Hours:
Monday thru Friday
8:30 AM – 4:30 PM

