TRIGGER THUMB & TRIGGER FINGER
Stenosing tenosynovitis can occur in the thumb or in any finger, and can even occur congenitally, in infants, but is most commonly present in people who either are developing a mild form of arthritis, already have rheumatoid arthritis or another kind of arthritis or have overused the tendon, so that the covering of the tendon has swollen, and gets caught in the pulley system.
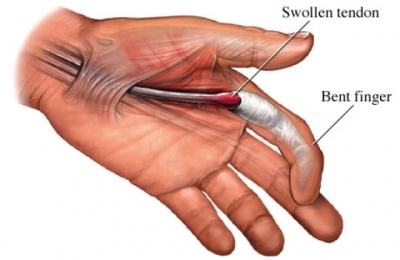
The tenosynovitis most commonly occurs in the ring or middle or long fingers, with inflammation of the metacarpal-phalangeal joint pulley causing a discrepancy between the size of the tendon and pulley. The tendon may become thickened just proximal to the pulley and this discrepancy in size can cause a snapping or locking phenomenon, holding the thumb or finger flexed or extended depending upon when the “nodule” gets caught, with reference to the pulley mechanism/ See drawing.
Often palpation or pressure of the flexor tendon over the MCP joint can be painful, as can the triggering be painful, and the triggering may get so severe that the thumb or finger gets locked in either flexion or extension, and must be, forcefully, passively, brought back to the flexed or extended position, using the other hand.
Etiology
This problem can be the result of repetitive pinching or gripping of the fingers or thumb, as in a cumulative trauma disorder, form ones’ work and/or hobbies or from the result of direct trauma.
If the triggering is congenital in origin (the patient is born with the triggering or it appears very soon after birth), and does not spontaneously disappear after the first couple of months, it will usually need to be released surgically, by enlarging the pulley-flexor sheath thickening.
Treatment
If the problem is developmental, it then will often respond to rest, avoidance of activities that cause the problem to arise, and taking of non-steroidal anti-inflammatory medication (including aspirin).
If these conservative methods are unsuccessful, and the problem persists, the trigger finger or thumb will occasionally respond to the injection of a local anesthetic and corticosteroid into the flexor sheath, utilizing a very small needle, and this should always be tried, prior to surgery, unless there is complete locking of the joint.
Since the injection of the steroid around the tendon sheath has a tendency to weaken the tendon for several days, if an injections is indicated, the involved finger will have to be protected from strenuous overuse for 10-20 days following the injection. If the triggering does not respond to the injections, following a maximum of 3 injections for safety’s sake, then surgical release is indicated. Also the injection should not be repeated any more frequently than every 3 – 4 weeks, up to a maximum of 3 injections.
Surgery
If surgery is indicated, it can usually be done utilizing either a wrist block or a local anesthetic, does not require general anesthetic, and is usually done on an outpatient basis.
The surgery, if done on a patient who does not have rheumatoid arthritis, simply consists of sectioning or dividing the pulley that is entrapping the tendon with a “nodule” in it. In patients with rheumatoid arthritis, the surgery is somewhat more complicated, and involves removing enough of the nodule to allow motion of the tendon within the pulley but the pulley itself is not sectioned, since this can increase the tendency, with patients with rheumatoid arthritis, to enhance the crookedness of the fingers.
For this latter reason, if more than one finger is involved, or if the problem is recurrent over several months period, blood tests are usually done to make sure the patient does not have rheumatoid arthritis, prior to any surgical procedures being done.
Following surgery, the hand involved is usually placed in a bulky dressing for a few days, after which the patient is encouraged to move the digit as much as possible, and the sutures are removed after 2-3 weeks. The patient will be requested not to get the incision site wet until after the sutures are removed, and will need to avoid heavy work for approximately 3-4 weeks following surgery.
Once full range of motion without pain or “sticking” is present, usually after 4-6 weeks, the patient may return to regular activities without restriction.
Contact Us
13710 Olive Boulevard (Primary Office)
Chesterfield, MO 63017
Telephone: 314-469-PAIN (7246)
Fax: 314-469-7251
Exchange: 314-441-6965 (for after-hour Emergencies Only)
Hours:
Monday thru Friday
8:30 AM – 4:30 PM