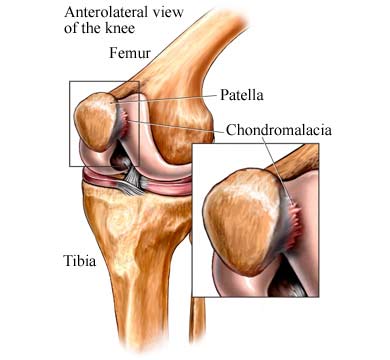
CHONDROMALACIA PATELLAE
Knee anatomy and Mechanics:
Three bones meet in the knee: the thighbone (femur), the shinbone (tibia), and the kneecap (patella). When the leg moves, the kneecap slides along a shallow groove in the femur known as the trochlear groove. The joint is cushioned and made smooth by articular cartilage, which wraps around the ends of all the bones in the joint. Repeated abnormal stress of the joint, whether due to age, injury, abnormal alignment or muscle weakness, can weaken and soften the articular cartilage. Doctors estimate that about one-half of all non-injury knee pain complaints are due to this disorder.
When afflicted with the condition, the patient’s knee rubs against the trochlear groove, instead of gliding smoothly across it. The damage may range from a slight abnormality of the surface of the cartilage to a surface that has been worn away completely to the bone. Anterior knee pain can present a diagnostic challenge because of the complex anatomy of the knee.
Note: There are other causes of anterior knee pain not considered here, which include scar tissue (plicae), patellar tendonitis and other soft tissue abnormalities.
Symptoms (Chondromalacia patellae):
- Pain in the front of the knee, especially when using stairs or climbing up or down hills
- Squatting, lunging
- Pain may radiate toward back of knee
- Cracking or grating in the knee
- Knee seems to “catch”
Cause and Risk Factors:
- Overuse when an abnormality exists
- Chronic Injury
- Muscle weakness (vastus medialis muscle)
Risk Factors:
- Risk factors include participation in high-impact sports like running, skiing, soccer and high-impact aerobics when a previous abnormality exists. These sports do not cause chondromalacia themselves. Trauma to the front of the knee can cause a cartilage injury.
- The Q-Angle, the angle formed by the thighbone and the patellar tendon, is also a major factor in the development of anterior knee pain syndrome.
- Quickly growing teenage women most often have a more acute Q-angle than others, and are thus at the highest risk group for developing the condition.
- Old age.
- Knock-kneed or bow-legged stance also increase the risk for developing anterior knee pain syndrome.
Treatment (Immediate care):
- Take aspirin or an anti-inflammatory medication, such as ibuprofen for a week.
- Avoid kneeling, climbing too many stairs, or sitting too long.
- Avoid jumping sports like basketball or volleyball.
- At your doctor’s advice, do low-impact exercises to strengthen the knee muscles. Your doctor may refer you to a therapist for exercises.
- Using knee supports can sometimes help avoid further injury.
- Call your knee specialist doctor if the following does not cure the symptoms.
Injections:
Cortisone injections can help reduce the inflammation within the joint capsule. It would be more beneficial to combine Physical therapy with injection therapy. Hyaluronate (often referred to as “Chicken shots”) injections can be helpful if the underlying cause is degenerative arthritis of the joint.
Surgical Procedures:
Surgery may be necessary in some cases. Your surgeon or physician may recommend arthroscopy surgery to assess the extent of the injury and smooth the surface of the cartilage. Other procedures to correct alignment of the kneecap may be undertaken simultaneously.
Prevention:
Check with your doctor before beginning any sport or exercise routine. Also, stay away from activities that require deep knee bending especially if you are at risk for chondromalacis patellae or already have low-grade knee symptoms. Physical therapy guided exercises are recommended which can be completed in either Illinois or St. Louis.
Strengthening Exercises:
The best exercises for chondromalacia patellae in St. Louis, tend to be those that focus on the hip (gluteal exercises) and flexibility exercises. An exercise that directly put force through the knee, especially the knee extension exercise is not appropriate and usually painful. Swimming is a good overall exercise.
A more specific exercise, for example, is what we call the lateral “monster walk. “ This requires a 20-inch piece of thick theraband or tubing tied in a circle and wrapped around both ankles. The patient will stand with his feet shoulder-width apart (never let the feet get any closer than that) and he walks sideways across the floor against the resistance of the band. The knees should be slightly bent; the buttocks should be down and back. Stress should be felt in the quadriceps and in the gluteal muscles. Repeat 10 steps in each direction, 2-3 times. Bicycling can sometimes be an irritant for chondromalacia in some people, but in others it can be a very good exercise. Do not do it or any exercise, if it reproduces your pain.
Contact Us
13710 Olive Boulevard (Primary Office)
Chesterfield, MO 63017
Telephone: 314-469-PAIN (7246)
Fax: 314-469-7251
Exchange: 314-441-6965 (for after-hour Emergencies Only)
Hours:
Monday thru Friday
8:30 AM – 4:30 PM